Ivy Blog
Re-Thinking Brain Tumor Drug Development
- November 9, 2020
- Nader Sanai
- Posted in Glioblastoma
Originally published in IBTA’s Brain Tumour Magazine: World Edition 2020/2021
Recently, new cancer drugs have generated notable successes in tumor control. For patients with advanced lung or skin cancer, for example, a growing arsenal of approved therapeutics are yielding historical improvements in survival. Why has this surge in successful drug development not yet touched the brain tumor community? At least part of the reason has to do with our ability to translate a successful result from the brain tumor laboratory to the brain tumor patient.
Drug development typically begins with ‘preclinical’ studies that experimentally treat animals harboring brain tumors. These tumors are generated from genetic manipulation of the animal or direct injection of a human tumor into an animal’s brain. A more simplified approach to drug testing entails treating brain tumor cells or lumps of human brain tumor tissue in a Petri dish. At best, these models are loose approximations of a patient’s reality. Thus, it is no surprise that laboratory studies have never accurately predicted the results of human brain tumor clinical trials.
Breaching the blood-brain barrier and other pillars of resistance
But replicating the complexities of a human brain tumor in the laboratory is not the only front in this war. For its own protection, the brain is designed to keep things out. This self-defense mechanism, enabled by the ‘blood-brain barrier,’ is why drugs effective for other human ailments are, thankfully, not detrimental for the brain. In fact, 99% of all new drugs are incapable of crossing the blood-brain barrier. Identifying which new drugs have the potential to gain access to brain tumors is a matter of chemistry. The challenge, however, lies in recognizing which drugs actually succeed at this in patients.
The most common method of estimating a new drug’s capacity for human brain penetration is to administer the drug to an animal and then measure its concentration in the animal’s brain and brain tumor tissue. Unfortunately, the assumption that these results will represent the human experience is fraught with risk. Specifically, the blood-brain barrier is assembled differently for every species. So, what penetrates the mouse brain does not necessarily penetrate the human brain. Beyond this structural issue, there is the issue of drug metabolism. Each species processes drugs differently, which means an identical dose (adjusted by body weight) for a mouse and a human can yield two divergent results.

Phoenix, Arizona, United States
A final pillar of resistance for brain tumors is their diversity. For many other cancers, the biology of each tumor type is very similar from patient to patient. Skin cancer, for example, can be subcategorized into different genetic subtypes, but within each subtype, there is little variation between patients. Brain cancers are far more fluid. Within each patient, tumors are continuously reorganizing with hyper-evolutionary speed. This not only creates a moving target, but it means two patients with exactly the same tumor type and treatment can have wildly different outcomes. In the context of a clinical trial, this adds substantial complexity to identifying drugs that ‘work.’
Drug development for non-brain cancers does not face such harrowing obstacles. Animal models for lung and skin cancer are reliable proxies for the human version. Drug delivery to human lung and skin cancer is not an issue. In contrast, for glioblastoma—the most common brain cancer and deadliest cancer known to man—these realities are central to the drought in new drug development. Worldwide, it has been 20 years since a new drug approval has provided glioblastoma patients with a survival benefit.
The Phase 0 Clinical Trial
The brain cancer community is readying its response. Drug discovery and medicinal chemistry are now in an era of unprecedented productivity and innovation. The pharmaceutical and biotech industries are blossoming, driving the creation of new drugs and new drug companies at a record pace. In 2010, the US FDA approved 21 new drugs, yet in 2019, they approved 48. By all indications, the tide will continue to rise as we enter a new decade.
The rush of new experimental drugs for brain tumors, however, still faces the same obstacles outlined above. A more efficient and predictive system for testing is needed. Fortunately, we can borrow a strategy from the medical oncology playbook—the Phase 0 clinical trial. For years, Phase 0 clinical trials have enabled medical oncologists to rapidly identify which new therapies warrant accelerated development and, equally importantly, which new therapies are destined for failure. This specialized strategy for clinical trialing saves both time and money—two commodities the brain tumor community has in short supply.
assess whether a new drug combination is ready for a
first-in-human Phase 0 clinical trial using a patient-
derived animal brain tumor model
In its simplest form, a Phase 0 clinical trial asks the same questions that we ask in animal models, except it does so in humans. After administering a small amount of an experimental drug to a patient before planned sampling of the patient’s tumor tissue, two critical questions can be answered: (1) Does the new drug reach the patient’s tumor in sufficient concentration? (2) Does the new drug hit its intended molecular target in the patient’s tumor? In technical terms, the first question assesses the drug’s ‘pharmacokinetics,’ the second question assesses the drug’s ‘pharmacodynamics.’
For tumors like lung or skin cancer, Phase 0 clinical trials are comparatively straightforward to perform. Because these tumors have no blood-brain barrier, the patient can undergo a simple needle or shave biopsy on Day 1, a single ‘microdose’ of the experimental drug on Day 2, and another biopsy on Day 3. The trials are fast (the biopsies can be performed as an outpatient) and low-risk (the drug dose is exceedingly low).

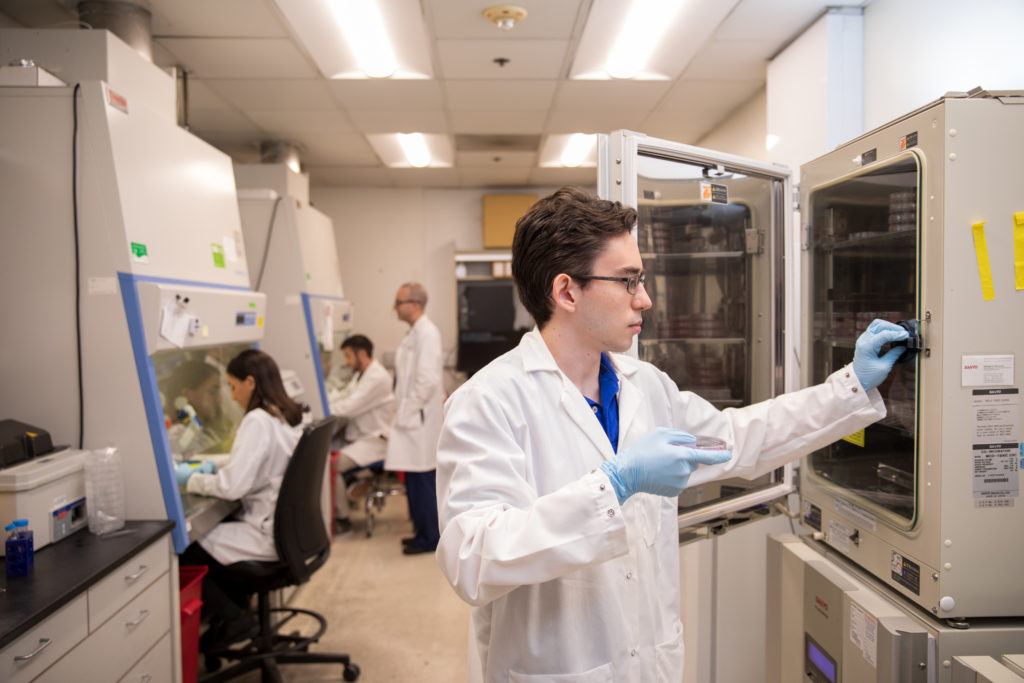
tumor patients, postdoctoral fellows in the Ivy Center’s
pharmacodynamics core perform an antibody test to measure
a drug’s effect in a Phase 0 trial patient’s tumor.
For brain tumor patients, however, things are never as simple. Even a biopsy requires drilling through the skull, and a drug ‘microdose’ is unlikely to traverse the blood-brain barrier. These added complications, however, pale in comparison to something else that brain tumor patients are missing: time. Today, the average glioblastoma patient survives for fewer than two years. The Phase 0 clinical trial, as described above, provides many things, including invaluable human pharmacokinetic and pharmacodynamic data essential for intelligent drug development, but it does not provide any hope of a therapeutic benefit for the charitable cancer patient who selflessly enrolls in such a trial. This not only makes it more difficult to fill the trials but, more importantly, it does not provide trial patients with a new therapeutic option.
The Ivy Brain Tumor Center in Phoenix, Arizona
In 2018, the Ben & Catherine Ivy Foundation awarded a $50M grant to establish the Ivy Brain Tumor Center at the Barrow Neurological Institute in Phoenix, Arizona. This not-for-profit, early-phase clinical trials program resides within an academic medical center that operates on over 1,200 brain tumor patients per year. Its sole focus is to adapt the Phase 0 clinical trial concept for these patients. For most Ivy Center Phase 0 trial patients, their journey begins at the time of tumor recurrence, when no proven therapeutic option exists. Based on a match with individual tumor genetics, an experimental drug cocktail is administered for several days prior to a planned craniotomy. For each patient, surgically sampled tumor tissue is assessed for drug penetration and target modulation. Within days of the operation, we learn whether the regimen will be effective in the patient and, if the answer is ‘yes,’ the patient continues with treatment. If the answer is ‘no,’ we have learned critical information without costing the patient an opportunity to pivot to another therapy or clinical trial. Importantly, this Phase 0 trial approach is individualized. Every patient’s response to an experimental drug is evaluated in the context of each tumor’s individual biology—success or failure is based on direct evidence of pharmacokinetic and pharmacodynamic response.
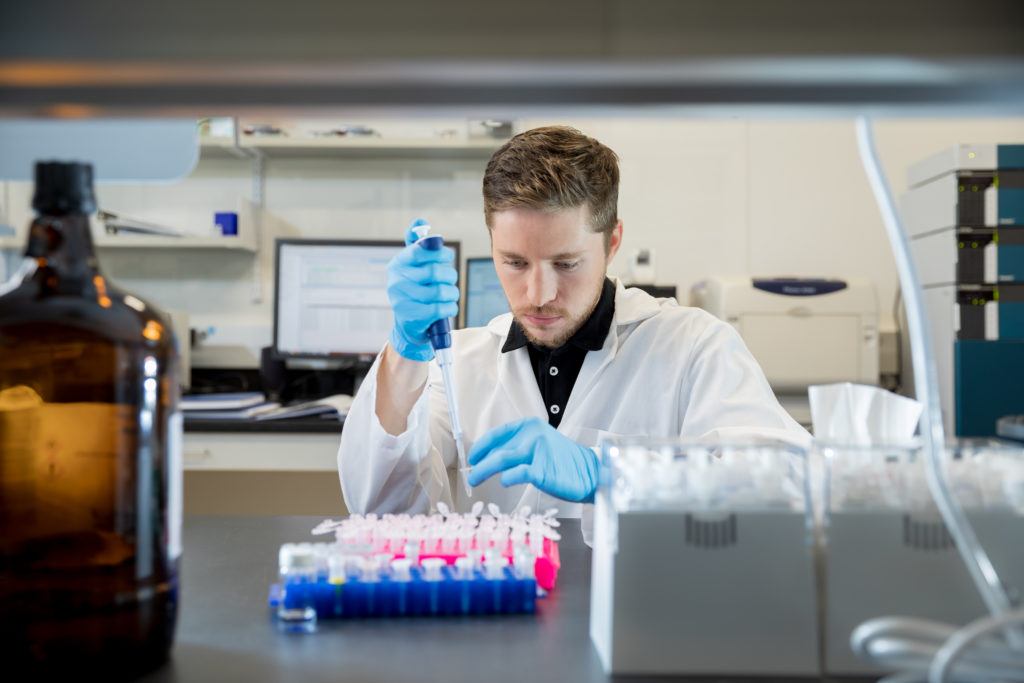
core prepares a patient’s tissue sample to determine if a
new, experimental drug cocktail has penetrated the
patient’s blood-brain barrier and reached the tumor in
sufficient concentrations.
Innovations to clinical trial design alone cannot move the needle unless we have access to suitable new drug combinations. To this end, the Ivy Center has adopted an aggressive stance in its pharmaceutical and biotech partnerships. Traditionally, the marriage between an academic medical center and a drug company is contentious. Details surrounding financial support, intellectual property, and contracting can plague even the best-intentioned projects, slowing progress to a crawl. A brain tumor clinical trial can take years to complete. To sidestep these landmines, the Ivy Center never requests a penny (from patients or industry) for its clinical trials, nor does it lay claim to intellectual property or downstream revenue. By assembling a specialized, stand-alone legal team unencumbered by the corporate policies of an academic medical center, the lead-in time for planning a new clinical trial can be measured in weeks. With this positive approach to industry partnerships, companies are incentivized to engage the brain tumor market.
Through hard-fought advances in the science and medicine of brain tumor patient care, our community of patients, physicians, caregivers, and scientists is approaching an inflection point. Successful drug development campaigns against other cancers provide a blueprint for efficient bench-to-bedside translation and effective industry collaboration. The Ivy Brain Tumor Center is carving a new road towards accelerated drug development and tailored care for individuals struggling against a perennially mortal adversary.